DEvelopmental anomalies of oral cavity : soft tissue structures
Introduction
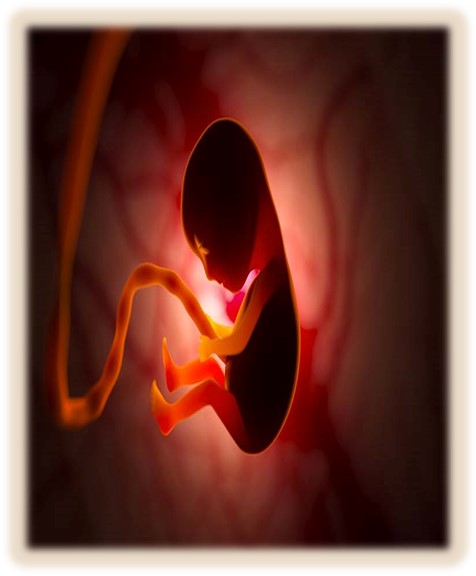
- Malformation or defects resulting from disturbance of growth & development are known as developmental anomalies .
- Manifestation of defects is evident either at birth or some times after birth
- Congenital anomalies of the oral cavity are structural abnormalities that occur during fetal development. These anomalies can affect the lips, tongue, palate, teeth, and other structures of the mouth.
Developmental disturbance of Jaws
1. Anathia

- Is a lethal anomaly characterized by absence of mandible & abnormally positioned ears.
- Autosomal Recessive mode of inheritance.
- More commonly, only a portion of one jaw is missing.
- In maxilla – maybe one maxillary process or even the premaxilla.
- DEvelopmental anomalies of jaw
- Partial absence of the mandible is even more common.
- Pathogenesis:
- • Failure of migration of neural crest mesenchyme into the maxillary prominence at the fourth to fifth week of gestation
- •The prognosis of this condition is very poor and considered to be lethal.
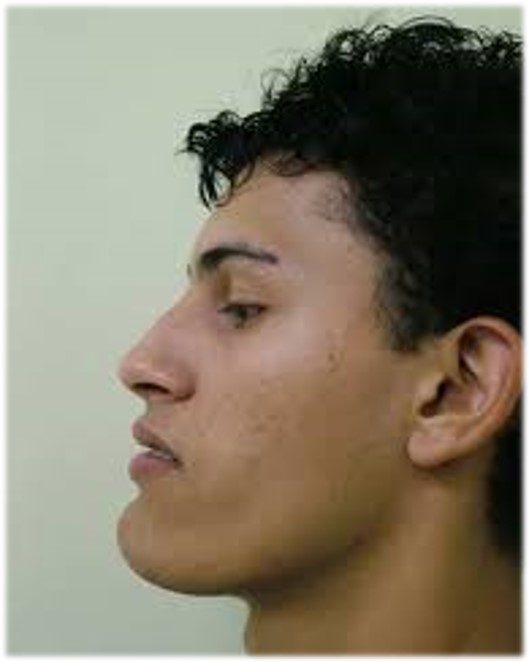
2. Micrognathia
- It refers to small jaw
- Either the maxilla or mandible may be affected
- 1.Congenital
- 2.Acquired
1. Congenital type:
- Unknown etiology.
- Associated with other congenital abnormalities like congenital heart disease and the Pierre robin syndrome.
2.Acquired type:
- Results from disturbance in the area of the temporomandibular joint .
- Clinical features
- severe retrusion of the chin , steep mandibular angle and deficient chin button.
Maxillary Micrognathia: –
- Frequently occur due to a deficiency in the premaxillary area .
- Middle third of the face retracted.
- Suggested cause mouth-breathing
Mandibular micrognathia:
Severe retrusion of chin and steep mandibular angle
3. Macrognathia
- It refers to large jaw
▪ Mandibular prognathism
- ✓ unknown etiology, some cases follow hereditary patterns.
- ✓ In many instances prognathism is due to disparity in the size of the maxilla in relation to mandible
- ✓ In other cases mandible is measurably larger .
Conditions which favor mandibular prognathism are:
- 1.Increased height of the ramus
- 2.Increased mandibular body length
- 3.Decreased maxillary length
- 4.Prominent chin
- 5.Posterior positioning of the maxilla in relation to the cranium
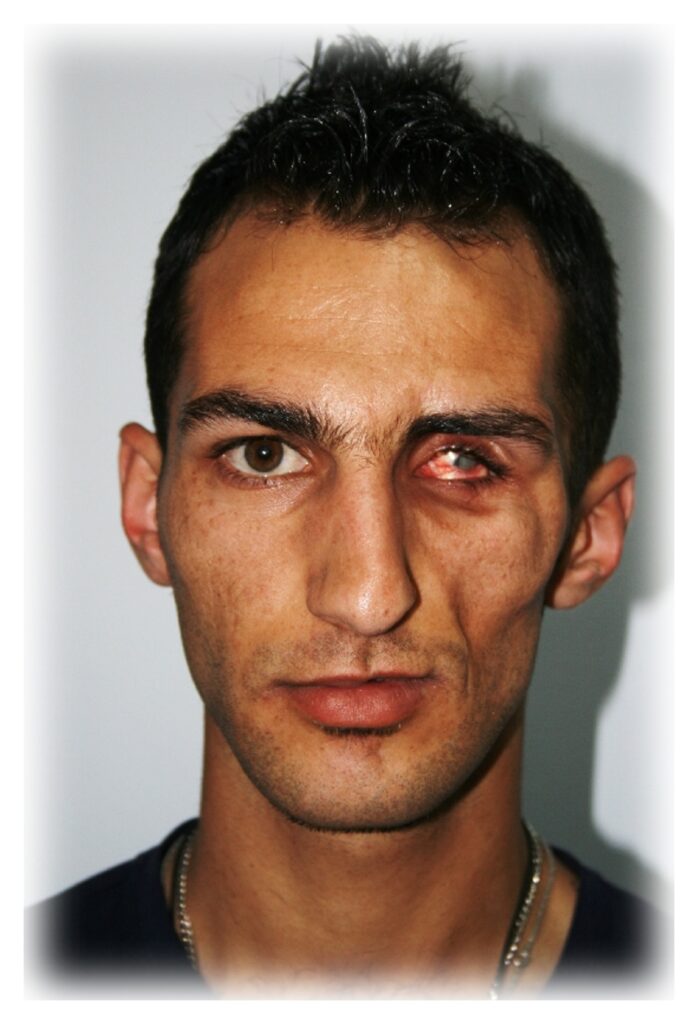
4. Facial hemihypertrophy

- •It is a rare developmental anomaly characterized by asymmetric overgrowth of one or more body parts.
- • It actually represents a hyperplasia of the tissue
- Etiology:
- •Unknown
- •Vascular or lymphatic abnormalities, CNS disturbances, Chromosomal abnormalities.
- Clinical Features:
- •F>M
- • Enlargement confined to one side of the body, Unilateral macroglossia, Premature development and eruption of teeth.
- • Increased size of dentition.
- Treatment :
- •Cosmetic surgery after cessation of growth
5. Facial Hemiatrophy
- Slowly progressive atrophy of the soft tissues on one half of the face.
- Characterized by Progressive wasting of subcutaneous fat, accompanied by atrophy of skin, cartilage, bone, muscle
- Occasionally spread to neck and one side of the body
- Rare condition
- Form of localized scleroderma
- Slowly progressive atrophy of the soft tissues on one half of the face.
- Characterized by Progressive wasting of subcutaneous fat, accompanied by atrophy of skin, cartilage, bone, muscle
- Occasionally spread to neck and one side of the body
- •Rare condition
- •Form of localized scleroderma
Developmental disturbance of Lip and Palate
1. Congenital lip pit
- Malformation of lip
- DEvelopmental anomalies of lip
- Hereditary pattern usually
- May occur alone or in association with other developmental anomalies like oral clefts
- Etiology:
- Notching of the lips at an early stage of development, with fixation of the tissue at the base of the notch /Failure of complete union of the embryonic lateral sulci of the lip
- Clinical features:
- Lip pit or fistula: Unilateral/bilateral depression, more common on the lower lip
- Lips sometimes appear swollen
- Commissural pits appear at the corner of the mouth on vermilion surface, preauricular pits may be seen
- Sparse mucous secretions may exude from the base of the pit
- Treatment:
- Surgical excision
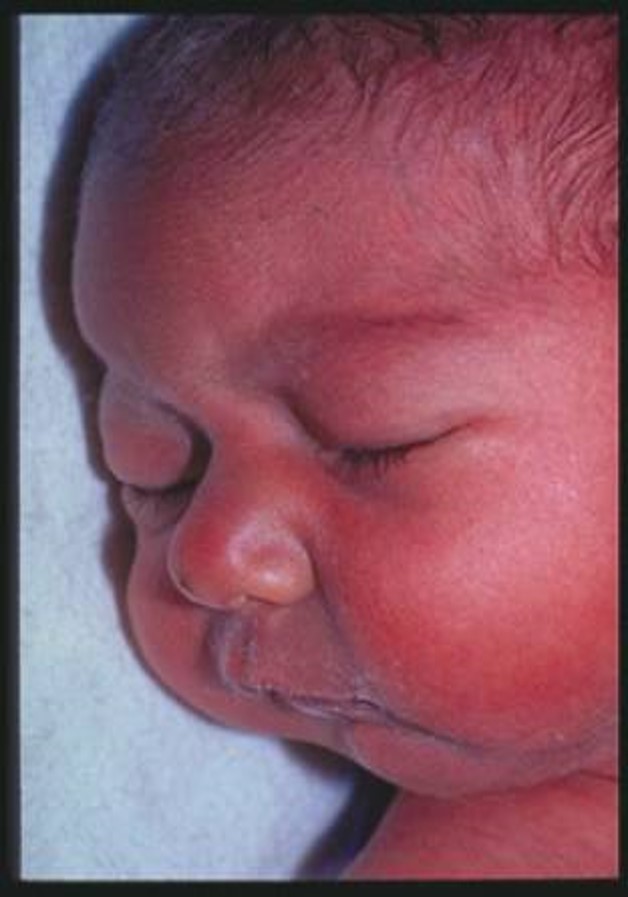
2. Cleft lip and palate

- Congenital malformations
- Two types of malformations : –
- 1. Cleft lip with cleft palate
- 2. Cleft lip with or without cleft palate Embryogenesis of lip & palate: 4th -12th week of gestation, failure of fusion of different processes leads to clefts.
- Pathogenesis:
- Caused by incomplete fusion of nasomedial or intermaxillary process during second month of embryonic development
- Predisposing factors:
- Hereditary/Environmental factors/Genetic causes
- Nutritional disturbances (insufficient evidence)/Stress: Increase cortisone
- Physiological, Emotional, Traumatic
- Other factors:
- Defective vascular supply to involved area,
- Mechanical disturbance (macroglossia) preventing fusion of parts, Circulating substances like drugs, toxins, alcohol, Infections, Lack of inherent developmental force
- CL + CP > M;
- Isolated CP > F
- Clefts divided into :-
- ✓ Syndromic: individuals with additional birth defects.
- ✓ Non Syndromic: affected individuals with no physical or developmental anomalies.
- ▪ Cleft lip can be:
- ✓ Unilateral
- ✓ Bilateral
- ✓ Cleft lip associated with alveolus, primary & secondary palate, soft palate
- Presenting Features:
- •Difficulty – eating & drinking because of nasal regurgitation of food and drinks.
- •Difficulty in speech, Mental trauma, Retrusion of maxilla with narrow upper arch resulting in the upper canines and premolars of affected side to be in lingual occlusion with mandibular teeth, Upper anterior may be malplaced / deformed or impacted, Repeated ear infections.
Treatment:

- Cleft lip repair should be accomplished during early infancy when child is stable:
- Rule of 3 tens:
- ✓ 10 weeks old,
- ✓ 10lb weight,
- ✓ Hb level of 10 g/dl
- •In later life, cheiloplasty is required.
- •Orthodontic treatment recommended and surgically placed orthopedic devices used in infants.
- •Closure of cleft palate defects with sliding and pharyngeal flaps by 1 year of age to promote normal speech. Palatal obturators for patient having difficulty in feeding, eating or drinking.
- •Early audiologic and speech evaluation.
- •Preventive dental services provided to the patient.
- •Plastic surgery procedure to correct aesthetics, function of vermilion border, lip, nose anticipated.
- •For child’s psychology and development, psychiatric consulted
3. Cheilitis glandularis

Deeply suppurative, chronic inflammatory condition of lower lip characterized by mucopurulent exudates from ductal orifices of labial minor salivary gland.
Progressive enlargement & eversion of lower labial mucosa.
Results in obliteration of mucosal-vermilion interface
Labial mucosal membrane is secondarily altered by environmental influences, leading to erosion, ulcerations and crusting
Etiology:
Chronic irritation
Unusual repeated manipulation including self inflicted biting or other trauma
Excessive wetting from compulsive licking
Lip enlargement due to inflammation, hyperemia, edema, and fibrosis
Surface keratosis & erosion due to long standing actinic exposure
Clinical Features:
•Lip swelling
•Burning discomfort or a sensation of rawness
•Dysplastic surface epithelial change
•Especially in fair skinned individuals with skin damaged skin
4. Chelitis granulomatosa
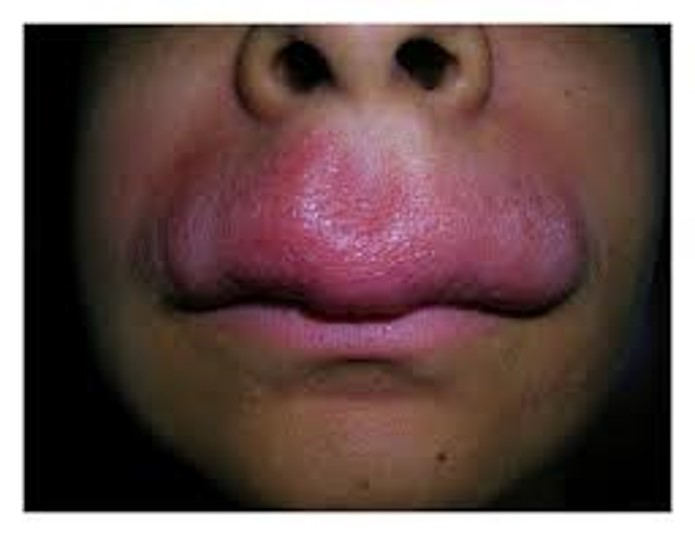
- Also called as Miescher-Melkersson-Rosenthal syndrome.
- Chronic swelling of the lip due to granulomatous inflammation
- Etiology:
- ✓ Genetic predisposition,
- ✓ Crohn disease,
- ✓ Sarcoidosis,
- ✓ Orofacial granulomatosa,
- ✓ Dietary habits,
- ✓ Contact antigens
- Clinical Features:
- •Non tender nodular swelling and enlargement of one or both lips
- •Accompanied by fever and mild constitutional symptoms like visual disturbances, headache
- •Enlarged lip appears cracked and fissured with reddish brown discoloration and scaling
- •Fissured lips painful and acquire firm rubbery consistency
- •Fissured tongue, loss of taste sensation, decreased salivary gland secretion.
- Treatment:
- Patch test to exclude reactions to metals, food or other oral antigens.
- Intralesional corticosteroids, non steroidal anti-inflammatory agents, mast cell stabilizers, clofazimine, tetracycline.
- Surgery and radiations.
Developmental disturbance of Oral mucosa
1. Fordyce granules

- Heterotrophic collection of sebaceous glands in oral mucosa
- DEvelopmental anomalies of oral mucosa
- Clinical Presentation:
- ✓ Small, yellow plaques on the mucosa
- ✓ Bilaterally symmetrical on cheeks
- ✓ Other sites: Retromolar region, mucosa of lips
- ✓ Rare – tongue, gingiva, palate & frenum
- Clinical Features
- ✓ Normal sebaceous glands without hair follicles
- ✓ Focal Epithelial Hyperplasia
- ✓ Contagious
- ✓ Young / Middle aged
- ✓ Labial, lingual, buccal mucosa
- ✓ Lesions: Papillary/smooth flat top, papules, plaques, cobble stone or fissured appearance
- ✓ Mucosa 8-10 times thicker
- Treatment
- ✓ Conservative surgical excision
- ✓ Maybe an oral manifestation of AIDS
Developmental disturbance of Gingiva
1. Fibromatosis Gingivae

- Diffuse fibrous overgrowth of gingival tissues
- Majority of cases – Heredity
- Association with hypertrichosis seen
- DEvelopmental anomalies of gingiva
- Clinical Features
- Birth or young children
- Firm, dense, non painful diffuse, smooth or nodular enlargements of gingiva, pale color
- Crowns of teeth may be hidden or eruption prevented
- Treatment:
- Surgical excision
- In some cases tooth extraction alone causes its shrinking
Developmental disturbance of Tongue
1. Aglossia & Microglossia

- Very rare Developmental anomalies of tongue
- Absence of tongue or presence of rudimentary tongue
- Usually associated with malformations in the extremities
- Difficulties due to the limited functions of the tongue
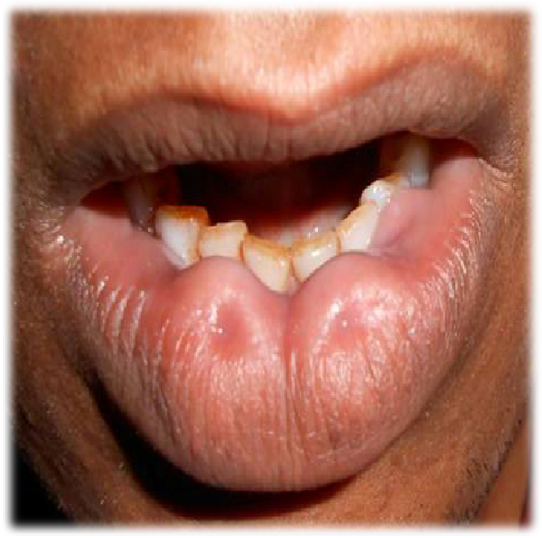
2. MACROGLOSSIA

- Enlargement of tongue
- Relatively uncommon disorder
- Etiology:
- Generalized and Localized
- Localized:
- ✓ Congenital – Hemangioma, Lymphangioma and Lingual thyroid
- ✓ Inflammatory – Tuberculosis, Actinomycosis, Dental infection, Syphilitic gumma, Riga disease, Ranula, and Sublingual calculus
- ✓ Traumatic -Dental irritation, Hematoma, and Postoperative edema
- ✓ Neoplastic lesions Malignant- Carcinoma and Sarcoma Benign – Granular cell tumor, Neurofibroma, Leiomyoma and Lipoma.
- Generalized:
- ✓ Congenital – Primary idiopathic macroglossia, Cretinism, Hemangioma, Lymphangioma
- ✓ Inflammatory – Chronic glossitis
- ✓ Traumatic – Postoperative edema
- ✓ Metabolic -Myxedema, Amyloidosis, Lipoid proteinosis, Steroid therapy, and Acromegaly
- Clinical Significance
- ✓ Tongue protrusion
- ✓ Noisy breathing,
- ✓ Speech impairment,
- ✓ Swallowing difficulties,
- ✓ Drooling of saliva
- ✓ Airway obstruction
- Treatment:
- ✓ Successful treatment require appropriate rehabilitation and long term follow up.
- ✓ Treatment options varies from observation, orofacial therapy and surgery.
- ✓ In adults the initial treatment should be conservative but main treatment is partial glossectomy.
2. ANKYLOGLOSSIA

- Ankyloglossia / Short frenum / Short frenulum / Tongue tie
- Restricted lingual frenum – Reduced mobility of the tongue
- Ankyloglossia occurs as a result of the fusion of the lingual frenum to the floor of the mouth.
- Partial ankyloglossia or “tongue-tie” is a much more common condition, because complete fusion rarely occurs.
- This leads to a myriad of speech problems such as lisping and stuttering, periodontal and swallowing problems and dental problems such as gap between mandibular incisors
- Treatment
- If necessary, tongue-tie can be treated with a surgical cut to release the frenulum (frenotomy)
3. CLEFT TONGUE

- Cleft tongue is a condition where the tongue has a cleft running right across in the center of the tongue anterio posteriorly.
- Complete clefting (Diglossia) is extremely rare and occurs as a result of lack of developmental forces to push both halves of the tongue towards each other.
- Partial clefting presents as a deep groove in the middle of the tongue and is a common feature in the oro-facial-digital syndrome (thick fibrous bands in lower anterior mucobuccal fold and clefting of hypoplastic mandibular alveolar process).
- Bifid tongue in association with Klippel-Feil anomaly and cleft palate has been reported.
- Cleft tongue is of little importance other than causing difficulty in eating as food gets stuck in the cleft causing irritation.
4. FISSURED TONGUE
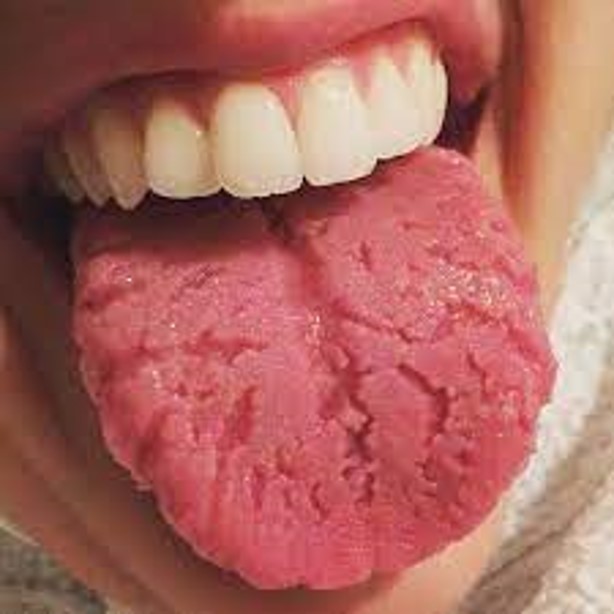
- ✓ Grooves with varying depths along the dorsal and lateral aspects of the tongue.
- ✓ The depth of the fissures varies, up to 6 mm ✓ The fissures or grooves may be interconnected, separating the tongue dorsum into several lobules.
- ✓ Definitive etiology is unknown of this Developmental anomalies .
- ✓ In some cases, associated with infection or malnutrition or benign migratory glossitis .
- Histology:
- ✓ Hyperplasia of retepegs.
- ✓ Loss of keratin hairs on surface of filliform papilla.
- ✓ Papillas are seperated by deep grooves.
- ✓ Micro abscesses in upper epithelial layers and poly morpho nuclear infiltrate into epithelium.
- ✓ Mixed inflammatory infiltrate in the lamina propria.
- Treatment
- ✓ No specific treatment required.
- ✓ Patients should be advised to brush tongue since grooves may act as a source of bacterial accumulation and cause irritation
5. GEOGROPHIC TONGUE

- Benign condition, occurs in about 3% of the general population
- Etiology & pathogenesis
- ✓ Poorly understood
- ✓ May be hypersensitivity or environmental or hormonal factors
- Although this is an inflammatory condition histologically, a polygenic mode of inheritance has been suggested because it is seen clustering in families.
- Clinical features
- ✓ It can affect all age groups, Adults>Children
- ✓ Females twice greater than Males
- ✓ Burning sensation or irritation of the tongue with hot or spicy foods Classic manifestation: Area of erythema, with atrophy of the filiform papillae of the tongue, surrounded by a serpiginous, white, hyperkeratotic border.
- ✓ Primarily affects the dorsum and often extending to involve the lateral borders of the tongue.
- ✓ Similar lesions may be present concurrently on other aspects of the tongue or other mucosal sites.
- Histology
- ✓ Microscopically it is described as a psoriasiform mucositis
- ✓ At the periphery, elongation of the rete ridges is noted with associated hyperparakeratosis and acanthosis
- ✓ Toward the center of the lesion, corresponding to the erythematous area clinically, loss of filiform papillae with migration and clustering of neutrophils within the epithelium
- Treatment
- ✓ No medical intervention is required because the lesion is benign and most often asymptomatic.
6. MEDIAN RHOMBOID GLOSSITIS

- Median rhomboid glossitis / Central Papillary Atrophy /Posterior Lingual Papillary Atrophy
- Focal area of susceptibility to recurring or chronic atrophic candidiasis.
- Etiology
- During this period of fusion posterior dorsal point of fusion is occasionally defective, leaving a rhomboid-shaped, smooth erythematous mucosa lacking in papillae or taste buds derived
- Clinical features
- ✓ The lesion is found in one of every 300-2,000 adults
- ✓ Shows 3:1 male predilection.
- ✓ Presents in the posterior midline of the dorsum of the tongue, just anterior to the V-shaped grouping of the circumvallate papillae.
- ✓ The long axis of the rhomboid or oval area of red depapillation is in the anterior-posterior direction.
- ✓ Erythematous clinical appearance
- ✓ Typical lesions are less than 2 cm. in greatest dimension
- ✓ Most demonstrate a smooth, flat surface, sometimes surface may be lobulated
- Treatment
- ✓ No treatment is necessary for median rhomboid glossitis, but nodular cases are often removed for microscopic evaluation.
7. LINGUAL THYROID GLAND

- Accessory accumulation of thyroid tissue that is usually functional within the body of the posterior tongue
- Etiopathogenesis:
- ü Late in 1st month of IU life the anlage of the thyroid gland descends from the posterior dorsal midline of the tongue to its final position in the lower neck.
- ü If the embryonic gland does not descend normally, ectopic or residual thyroid tissue may be found between the foramen caecum and the epiglottis.
- Clinical features
- ✓ The lingual thyroid is four times more common in females than in males.
- ✓ It presents as an asymptomatic nodular mass of the posterior lingual midline, usually less than a centimeter in size but sometimes reaching more than 4 cm in size .
- ✓ Larger lesions can interfere with swallowing and breathing, but most patients are unaware of the mass at the time of diagnosis, which is usually in the teenage or young adult years
- Clinical features
- ✓ The lingual thyroid is four times more common in females than in males.
- ✓ It presents as an asymptomatic nodular mass of the posterior lingual midline, usually less than a centimeter in size but sometimes reaching more than 4 cm in size .
- ✓ Larger lesions can interfere with swallowing and breathing, but most patients are unaware of the mass at the time of diagnosis, which is usually in the teenage or young adult years
- Histology
- ✓ The lingual thyroid consists of a non-encapsulated collection of embryonic or mature thyroid follicles which may extend between muscle bundles, raising suspicions of malignant invasion.
- ✓ The follicular cells are normal or atrophic in appearance.
- Treatment
- ✓ Surgical excision or radioiodine therapy are effective treatments for lingual thyroid, but no treatment should be attempted until an 131 iodine radioisotope scan has determined that there is adequate thyroid tissue in the neck.
8. LINGUAL VARICOSITIES

- It is a dilated , tortuous vein which is often subjected to increased hydrostatic pressure but is poorly supported by surrounding tissue
- Clinical features
- Usually involves the lingual ranine viens
- involved veins appear red or purple shotlike clusters of vessels on the ventral surface and lateral borders of tongue as well as in the floor of the mouth
- Presence of lingual varices before the ages of 50 indicates premature ageing
- Treatment
- no specific treatment
9. HAIRY TONGUE

- TONGUE, LINGUA NIGRA, LINGUA VILLOSA
- Characterized by marked accumulation of keratin on filiform papillae of the dorsal surface resulting in a hair like appearance
- CLINICAL FEATURES
- Formation of a pigmented thick matted layer on the tongue surface, heavily coated with bacteria and fungi
- Hair like appearence
- Halitosis
- Irritation of tongue due to accumulation of food debris
- Candidal over growth may cause glossopyrosis ( burning tongue)
- Simply brushing the tongue with a toothbrush or using a commercially available tongue scraper is sufficient to remove elongated filiform papillae and retard the growth of additional ones
For more updates on dental blog do follow The tooth times
Do follow Trending curiosity for trending updates
Please follow Civil engineer academy for blog related to civil blogs
For vacation planning contact Bangalore Tour and Travel